The “state of the burbs” blog recently visited the Healing Garden and spoke to our Co-Directors of Integrative care, Brianne Carter and Christine Zinke, about what makes the Healing Garden unique for patients, families, and caregivers. We are pleased to share original content and photos below from this in-depth interview.
All content courtesy stateoftheburbs.com
———————————–
 Nestled in the woods of Harvard down a winding driveway through the trees is the Virginia Thurston Healing Garden. The magic of the Healing Garden starts with Virginia Thurston, whose gardens were her own joy and refuge during her struggle with breast cancer. Her support group of women was so close that when she was too sick to leave the house, they all came to her. It is that spirit of community and belonging that is carried on today in her sacred spaces.
Nestled in the woods of Harvard down a winding driveway through the trees is the Virginia Thurston Healing Garden. The magic of the Healing Garden starts with Virginia Thurston, whose gardens were her own joy and refuge during her struggle with breast cancer. Her support group of women was so close that when she was too sick to leave the house, they all came to her. It is that spirit of community and belonging that is carried on today in her sacred spaces.
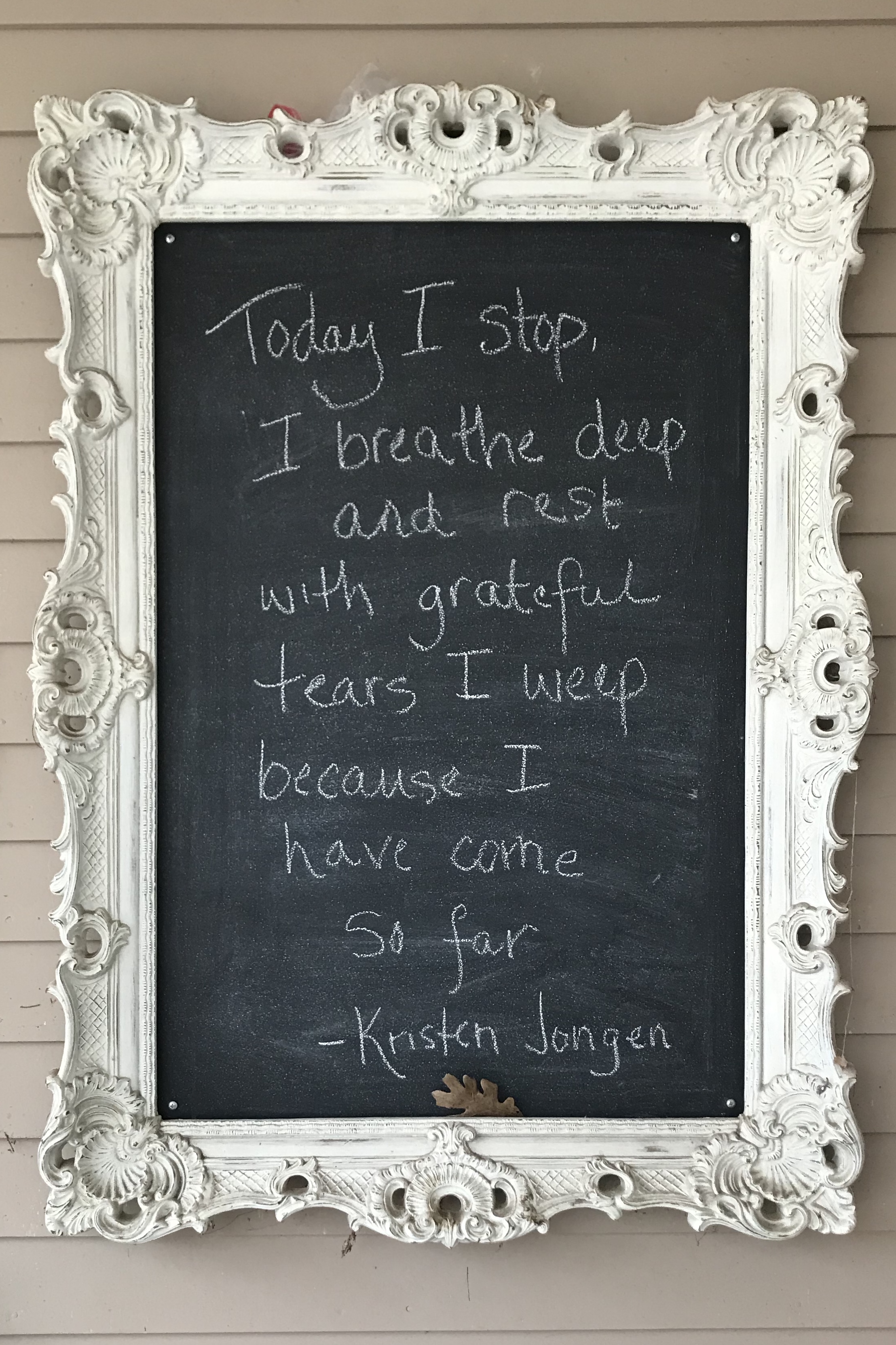
Virginia’s gardens are places of reflection and transformation for patients. A deep quiet escorts guests on a walk around the grounds. Senses become heightened as if you are at the entrance to introspection. Springtime at the Healing Garden serves as a perfect reminder of the bounty of resilience, growth, and change as the plants start to awaken. Solomon Seal’s arched stalks dot the shaded bank of the koi pond. Lilacs on the brink of blooming emit their lovely scent carried in the air through the waves of light breezes. As you make your way to the lower gardens, the experience is downright transformative. Flowering tree branches sway ethereally. Massive azalea bushes bloom in varying pinks. Guests are encouraged to sit at the fish pond on well-loved benches. Simply listen to the water as the frogs jump about.
Virginia’s cottage has been transformed into an integrative health center for healing and togetherness that has been guiding those affected by cancer since 2000. Patients meet for group sessions sitting in a circle, basking in the warmth of the sunroom. A wall of tea offers enticing options including golden milk and scoops of turmeric. The yoga instructor prepares for a morning session while visitors share homemade lemon bread as they wait for a massage or acupuncture appointment. Artwork of all kinds created by patients is displayed along the walls, reminding the viewer that we are complex characters with endless stories of love, loss, and hope. If you could imagine the most perfect place to embrace a loved one who is facing cancer, this is it.
We had the incredible opportunity to spend time with the Brianne Carter and Christine Zinke, the Co-Directors of Integrative Care at the Virginia Thurston Healing Garden, to talk about the invaluable work that is happening there, the power of togetherness in a community of others, and how we can help others heal.
SOTB: The Healing Garden is a fixture in the area that people recognize as a place where people with cancer can come to. But many in the community don’t necessarily know the wonder of what is actually happening here. What would you want the greater community to understand about the Healing

Garden?
Brianne: There is something about stepping onto the property. A lot of people say they hear about The Healing Garden, but it makes a difference to actually get here. This is a place to come if you have been affected by cancer, and you want to figure out how to move through it and how to live your life well. We are looking at how you can be with a community of others and get through this challenge with all the different dimensions of who you are.
Christine: Our serene setting helps deeply with that. It adds a whole other dimension to how you feel when coming in for treatments. Breathing and connecting to the environment here brings a level of peace to patients.

SOTB: A community of others, can you talk more about that?
Brianne: It’s having someone who gets it. We want people to feel looked at as a whole person, all the parts integrated. That is the other sense of community, being in a place where lots of others have walked through this, became healed, and lived well regardless of what happened with their illness.
Christine: It is so important to feel held and to know that people are walking alongside you. Even if you can’t verbalize all of that, sometimes it is just having people around you in silence, knowing you are not alone.

SOTB: The supportive therapies that you offer here are incredible: from yoga to massage, Qi Gong to expressive arts. What is the most popular?
Brianne: I’d say the most popular one is the cooking class.
SOTB: Really? That’s interesting.
Brianne: A lot of people in treatment are usually just getting through it, managing to eat whatever they can eat. But often, once treatment is over, eating is one of the things that you can control. A lot of people have gained weight from the steroids in the treatments; their digestion is wiped out, and the cooking class becomes almost an eating support group. People talk about tips and tricks and things that worked or didn’t work and share recipes. We have a chef who comes in and makes these delicious recipes that are super nutritious, easy to digest, and you get to eat it, which inspires everyone.
Christine: The clean eating piece is so important. The chef does such a wonderful job of promoting clean eating.
Brianne: People become so motivated. By virtue of the fact that they are regaining ownership of their bodies. Rather than it becoming overwhelming, it becomes inspiring. Which again, brings us to the idea of a community of others.
SOTB: And it’s food, people love food.
Christine: (laughter) Yes, well, there is also the coming together around food.
Brianne: Food had lost its thing for people, and now it can be taken back.
Christine: People who can take advantage of all the opportunities can really have an incredible day. Today I had a client who came in and did the yoga group. She had an appointment with me for individual therapy, and then she had a massage. So she was able to incorporate several sessions into one day.

SOTB: The Healing Garden welcomes people at all different stages of their journeys. Do you find people come back after a while?
Christine: Yes. We are inclusive to people at all different stages, and we have groups based on those differences. If you’re a talker and even if you aren’t, it can be just about listening. We have a treatment group, a bereavement group, people who are post-treatment, a client/caregiver group where everyone is together, a caregiver group, and a metastatic group. We really try to hit every stage of what is going on so that people don’t feel alone in that process.
SOTB: For clients and caregivers, it isn’t ever over, is it?
Christine: No, it’s not ever over. Living with the fear of recurrence for most people is extremely high. We find that a lot of people can compartmentalize as they are getting ready for their scans or appointments. But leading up to those appointments, their anxiety raises, and they are dealing with that fear.
SOTB: So you offer them the tools to navigate that experience. You also have a class for pre-surgery. Research suggests that people who take such a class exit the hospital earlier, have fifty percent less pain medication, and have a faster recovery.
Christine: Exactly. This is taking off, and people are gravitating toward that because they are now able to think, what is it they want their surgery to look like. What do they have to do to prepare for it, what do they want said to them when they are having anesthesia, what do they want said to them coming out of surgery.
SOTB: You are giving them leadership through visualization.
Christine: Yes, exactly. A sense of control is essential.

SOTB: Have you ever had a skeptical person who then leaves as a convert?
Brianne: Well, it’s a self-selective type of person who comes here in the first place. We work really hard at making this place feel accessible to folks who are more income insecure. In the intake process, we make sure that everyone understands that most people affected with cancer are either financially insecure or became so because you can go down to one income or no income. So this is a place that is not a luxury; it is a new way of life, and it is accessible to everyone. Some of the grants that we write are really to try to scoop in those who wouldn’t otherwise consider themselves belonging and accessing these kinds of supports. We just received a new grant to try to get transportation costs covered, because that is usually the primary variable for financially insecure people.

SOTB: It seems that for some, it is hard to say, “I’m sick.” What are your thoughts on that struggle to reveal?
Brianne: I think most of it is the stigma. You can get forced into an identity that you don’t want to have. But frankly, most people find that if you disclose that you are sick, others often forget rather quickly. It is just one of those things that it gets incorporated back in your life.
Christine: It is that sense of control again. This time in deciding who you are going to disclose to. There is a piece of being able to manage your sense of self and feeling that it is on your terms because when you have cancer, nothing is on your terms. There is the level of body betrayal, so to be able to feel that I am sharing with this person and not sharing with another, really gives people a sense of control.

SOTB: On that piece of disclosing, in thinking about the receiver, particularly friends. Friends don’t prepare for their friends to get sick. It isn’t something that we proactively do in the way we prepare for our parents getting older, for example. It is hard to know how to react, as it feels shocking. It seems that people can be really empathetic or unfortunately, people can be really thoughtless and say careless things. How can we be the best friend possible to someone sick?
Christine: Everyone has individual needs as to how they want it handled and how open they are in the process. So my thought is, first checking in to see what they need in the first place. Having that conversation with them. It may just mean that being a friend is just giving a phone call once in a while or it may mean needing to show up regularly.
Brianne: There is one woman who summed it up by saying, “I wish everyone would say, ‘ah that sucks, how can I help?’. Because she said, anyone who would go the cheerleading route or say ‘everything is going to be ok,’ none of it worked for her.
SOTB: That is a helpful piece of advice. You don’t want to overstep your boundaries, and you don’t want to step back and give too much space. So just speaking to your friend and saying, “What do you need from me?” is such a good direction.
Christine: Yes, absolutely, and it’s the understanding that people battling cancer may not know at that moment because they are so overwhelmed. They may not feel comfortable sharing, and asking for help can be really hard.

SOTB: How about the caregiver? It seems they are most often the one who forgets about their own care. What do you see as the biggest struggle for them, and what do you think caregivers need to be mindful of?
Brianne: I think that helplessness is the biggest challenge for caregivers. Watching a loved one suffer, and feeling incompetent is one of the most challenging pieces.
Christine: The desire to want to jump in and fix it when it’s not fixable is a piece of that helplessness. So many times, they are wrapped up in what they have to be doing because it is a constant job. They don’t realize that they need to take a break to re-energize. They can allow us to step into that role for a bit of time, and they can go and try to do something that makes them feel like them again.
Brianne: Statistically from the moment of diagnosis, a caregiver starts to contribute the equivalent of a 37 hour a week job. The distress level is higher in the caregiver for up to one year after treatment.
Christine: Everyone is so concerned about the person going through cancer, they don’t generally ask the caregiver, ‘how are you doing with all of this?’ They get overlooked in numerous ways.

SOTB: What have you learned about the human spirit from being here?
Christine: People are resilient. I realize there is a real desire to connect with others and not be alone in the process. I think in human nature not being alone, wanting to be held, and the desire to hold people even if you are going through the same thing. It is that connection and wanting that holding that just carries people through.
Brianne: I think there is a relief that can happen at times here around death being allowed to be in the room. Most of the time, we can live in a healthy level of denial in this culture around death. There really aren’t a lot of opportunities to talk about it. Here we can talk about it in a way that goes beyond the taboo of it. Everyone has had this opening of it in their lives, and their mortality is out there to contend with. When thinking about the human spirit, when you are forced to rip off that veil and look at death full on, there is this relief and an understanding that you’ve been fighting and resisting it. When you get to a point where you are not going to resist it, then you can learn to live better side by side with it, there is this deep breath that allows you to live more fully.
SOTB: What would Virginia think of what her garden has become?
Christine: I imagine that Virginia would be overwhelmed with gratitude for what the garden has transformed into. It is a dream come true, planting one small seed and having that bloom into a garden of hope for all to share. That could have only happened with many hands tending to the garden and planting their own seeds of memory and love.


This is so wonderful to read. You both touched on many key areas in dealing with cancer. Thank you for so clearly verbalizing the truth about the complexities in going through cancer.
Lovely piece! As a former client I always keep the healing garden and it’s staff (Betsy, Julie , Fran, Lana) and many others in my heart! It’s time to stop by and see the gardens in bloom!